HCMA and ICER – what did we learn?
by Lisa Salberg, Founder and CEO of the Hypertrophic Cardiomyopathy Association
11/30/2021
Of all the players in the healthcare system, patient advocacy organizations are often the most disadvantaged when a drug hits the market and they find themselves pitted against health providers, payers, pharmaceutical companies, and policymakers, all of whom want their piece of the financial pie. In my 25 years as the CEO and Founder of the Hypertrophic Cardiomyopathy Association (HCMA) this was never truer than during the last nine months while engaging with the Institute for Clinical and Economic Review (ICER) in their evaluation of the cost-effectiveness of a new drug, mavacamten.
Mavacamten is a first-in-class drug under review by the Food and Drug Administration (FDA) for the treatment of hypertrophic cardiomyopathy (HCM), a challenging cardiac condition that is relatively common but not well understood. Patients are often misdiagnosed which can delay treatment and exacerbate conditions such as shortness of breath, fainting, arrhythmias, and fatigue. Until mavacamten, HCM patients relied upon medications that were not tested nor labeled specifically for the condition leading to a plethora of “medication cocktails” that treat symptoms but not the underlying problem.
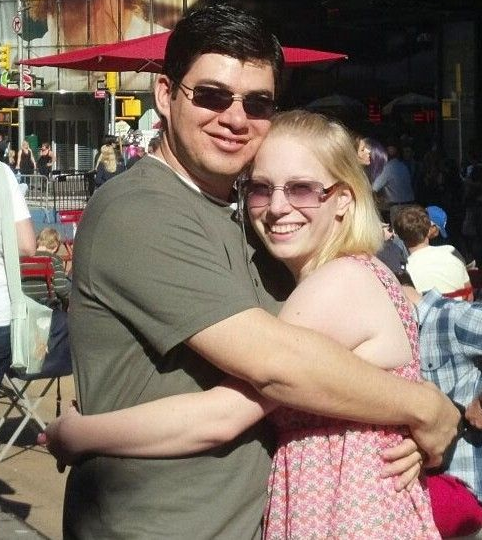
The HCM patient community is literally my family. I was diagnosed with the condition at the age of 12, lost my sister at the age of 36, lost my father when he was 73, and several other family members dating back to my grandfather who suffered a cardiac arrest at the age of 43 in 1953. Currently, eight family members are under a cardiologist’s care. Since forming HCMA, my goal has been to educate patients about the condition and ensure they have the best care possible. Until ICER’s decision to review the cost-effectiveness of mavacamten, HCMA had never faced the need to put a financial amount on what it meant to live a heart condition that varied to the point, for example, of putting some in the ER on a moment’s notice, others on disability, and others without access to insurance due to a pre-existing condition.
To say that patient advocacy organizations such as HCMA are ill-equipped to play a game of David & Goliath with ICER is an understatement. Never mind that ICER is a non-profit organization, independently funded with academic roots and doctorate expertise, the sheer inequity between HCMA’s resources and know-how and ICER’s parade of health economists, physicians, analysts, statisticians, lawyers, and health policy experts is an embarrassment to any claim that the process of evaluating mavacamten was fairly conducted.
To be clear, ICER’s claim that a cost-effectiveness analysis of a new drug will result in more reasonable and just coverage decisions by payers (and indirectly benefit patients and reduce healthcare spending for us all) is a laudable goal. But it’s the mountains of assumptions and hundreds of pages of economic modeling that leaves anyone involved with ICER with one simple question: how can ICER know so much about a drug the FDA has yet to approve for use?
Yes, I was part of the internal review committee and yes, HCM patients provided public comment and personal testimony at a public hearing. But while that ostensibly checks the box for patient engagement, it’s worth noting what it meant in easy-to-understand language. First, and most importantly, it meant a great deal of time. Over the course of the last nine months, I spent no less than 20 hours each week in conference calls with ICER, reviewing scoping documents, correcting statistics, deciphering tables and graphs, providing background materials, learning health economics, identifying clinical experts, consulting with outside economists, conferring with other national organizations, educating patients on the public comment process, identify gaps in data collection, appearing on “live” social media events, preparing videos of patients for a public hearing, talking to consultants, and debriefing the organization once the Final Report was issued.
Often my efforts were mired by statistics and terminology that were thrown around to describe the sheer nature of what I, and hundreds of thousands of other HCM patients, experience well beyond the medical bill that arrives in the mail. These ICER refers to as “contextual considerations” and are omitted from the official analyses due to their vague, difficult-to-measure quality. But they are hugely important to patients because they deal with such things as vocational choices, whether to have children, where to go to school, and the training needed for in-home care. All are factors that “cost” HCM patients dearly and yet my insistence that they be included fell short. The process was time time-consuming, tedious, and oftentimes, confrontational. None of this work was in the HCMA strategic plan for 2021.
Secondly, while fortunate to have Board members and HCM patients with professional expertise in health policy and reimbursement, their time alone required significant additional funding not in the organization’s budget for the year. Funds were also needed to prepare patients for public meetings, create surveys of insurance trends, hire consultants and writers, and ramp up communication and marketing efforts to educate patients through social media outlets and patient discussion groups.
ICER’s process moves at warp speed, and they did not slow down for an understaffed patient advocacy organization such as HCMA. It was an enormous commitment of time and money to participate effectively. As a small nonprofit, HCMA’s resources are limited, so every dollar and minute ICER demanded of me, or the organization was a dollar and minute taken from a patient in need of information and other responsibilities.
But most importantly, ICER’s review left an indelible impression on me that will resonate in the years to come as mavacamten enters the market – the undeniable truth that just because a new drug, with a promise of restored health exists, is no guarantee that it will be available to patients in need. With each document I reviewed and each hurdle I faced, I felt the weight of this reality facing the HCM community and wondered if my time was being well spent. Knowing ICER’s review could be misinterpreted or misused by health payers skittish about its value when whittled down to “quality-adjusted life years” sickened me.
In the end, however, I’m pleased that ICER clearly heard and incorporated many of HCMA’s perspectives in this assessment. They asked and we answered. Yet, our loss of time and the need for additional funds were unplanned for and have altered the plans for the organization significantly. Considering the drug is yet to be approved by the FDA and ICER’s evaluation relies on only one clinic trial comprised of 300 patients, it’s not difficult to conclude that it was based upon more assumptions than facts and has indelibly placed a monetary value on the unknown which may be hard to erase.
Unfortunately, patients are forced to navigate a complicated web of payer and provider priorities just to get treatment from a system that is ostensibly designed to serve them. While I appreciate that I was given a seat at the table, in the future I hope ICER will consider ways that make it easier for patients to engage, help patient advocacy organizations find funding and expertise to level the playing field, act only when sufficient data is available, and make investments in patient preference information and other outcomes data before making conclusions about the clinical or cost cost-effectiveness of treatment.
Getting access to high-quality treatment should not be this hard. Nor should it cost this much. We all have a role to play in patient-centered care.
The post Ever Wonder Who’s at the Center of Patient-Centered Care? Look Again appeared first on Hypertrophic Cardiomyopathy Association.

 Translate
Translate