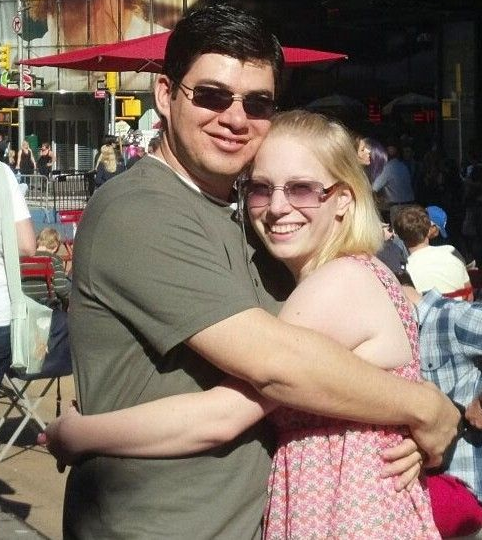
By Dawn Levitt – https://dawnlevittauthor.com/

My experience with the medical system began when I was a young child running around like most little kids do, but I became very short of breath and tired after a brief bit of exercise. My pediatrician diagnosed me with asthma and gave me an inhaler.
When I was seven years old, I collapsed while running laps in gym class. This was the 1970’s and I was sent to the principal’s office to wait for my mother to pick me up. She didn’t think anything of it because I had been a sickly child all my life, but my grandmother pushed for me to see the pediatrician. He detected a heart murmur and referred me to the Children’s Hospital of Detroit.
At the Children’s Hospital of Detroit, I was diagnosed with Idiopathic Hypertrophic Subaortic Stenosis (IHSS). This would later be classified as Hypertrophic Cardiomyopathy (HCM). As a child, I had no idea what that meant and neither did my mother. I was given beta-blockers and had to return once every summer for checkups.
At the age of 16, I was transferred to the care of a new cardiology practice opening in our small town. This new doctor never talked to me, the patient, but spoke with my mother. She didn’t understand most of what he told her, only telling me that I was not expected to live past the age of thirty years.
When I became an adult, I continued to see the same cardiologist who told my mother of my “expiration date” because he was the only cardiologist in town. Growing up with a heart condition, I had become used to regular doctor visits and always following doctor’s orders, so I never thought to question anything he said.
When I turned thirty and didn’t die, I began to think that the doctor might be wrong. My symptoms worsened, even with beta blockers and antiarrhythmic drugs, and the same cardiologist suggested I might need a pacemaker. Due to my absolute lack of understanding of my condition, I thought he was suggesting open heart surgery and balked at the idea. He referred me to another cardiologist at a larger practice who might be better equipped to help me.
This new cardiologist swapped some of my meds for a different combination and told me I didn’t need a pacemaker. But he never gave me any further information about my condition, and I never thought to ask. At my last appointment with him, he was not concerned about my worsening symptoms.
During that appointment, I told him about a recent business trip where I ran through the airport to catch my flight. During that run, I felt light-headed and like I was going to pass out. This was not a feeling I had experienced before. He asked if I felt any shortness of breath climbing stairs, and I told him that I did not. He was not concerned about the airport episode, instead noting that I had gained eight pounds since my last visit six months earlier.
“I think you would feel better if you lost ten pounds,” he told me. That was it. There was no echocardiogram, no blood work, no outpatient heart monitor. The nurse took my blood pressure and the doctor listened to my heart for thirty seconds.
Several weeks later, I came down with what I thought was the flu. It was the Christmas holiday weekend, and I went to the urgent care nearest my home. The doctor on duty confirmed the flu and prescribed Tamiflu. After Christmas, I followed up with my primary care physician because my cough had worsened. He diagnosed bronchitis. I returned to work after the New Year’s holiday, but I kept getting sicker, developing a worsening shortness of breath. This time, my primary care physician diagnosed pneumonia.
Two days later, I went to the emergency department at the hospital because I had reached the point that I could not breathe lying flat and even sitting up in the recliner to sleep had me struggling to draw a breath. I felt like I was drowning in dry air and began to panic.
It was the doctor at the emergency department who accurately diagnosed me with Congestive Heart Failure (CHF) and admitted me for treatment. After five days of receiving diuretics, several liters of fluid were removed from my body, and I could breathe freely again.
Even at this point, my understanding of my heart condition was sorely lacking. I falsely believed that the fluid removal had cured me. Unfortunately, I learned very quickly that the fluid was only one symptom of my underlying condition.
During this hospital admission, my original cardiologist came to my bedside. He was not surprised by the sudden failure of my heart, and he said the words I will never forget.
“This is the normal progression of your disease. Your heart will grow weaker until it stops. There is nothing more we can do for you.”
This was January of 2004, and the internet was still in its infancy. I read everything I could find about my heart condition and joined Yahoo Groups dedicated to CHF. One of the people I met online gave me the advice that saved my life. She told me to go to the Cleveland Clinic for a second opinion.
It was a stroke of luck that I was able to get an appointment at the Cleveland Clinic and it was there that I received an accurate diagnosis and a thorough plan of care. Just as important, they educated me on my condition and how to care for myself. They were the first medical providers to suggest a heart transplant for my condition.
I still had a long road ahead of me, but I had learned about my condition and how to advocate for myself. Without this, I would not be alive today. Always ask questions and push for answers. Don’t be afraid to seek a second opinion.
The post Educate and Advocate appeared first on Hypertrophic Cardiomyopathy Association.

 Translate
Translate